Can you die from long COVID? The answer is not so simple
Thursday, 14 November, 2024
By , ; , ; , ; , ; and ,
Nearly five years into the pandemic, COVID is feeling less central to our daily lives.
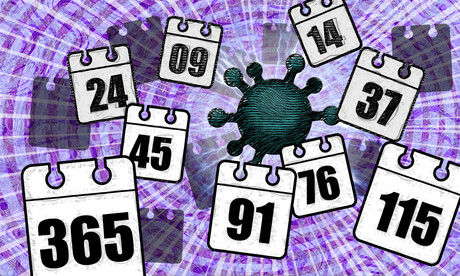
But the virus, SARS-CoV-2, is still around, and for many people the effects of an infection can be long-lasting. When symptoms persist for more than three months after the initial COVID infection, this is generally referred to as .
In September, Grammy-winning Brazilian musician died aged 83 after reportedly having long COVID.
show 196 deaths were due to the long-term effects of COVID from the beginning of the pandemic up to the end of July 2023.
In the United States, the Centers for Disease Control and Prevention reported 3544 from the start of the pandemic up to the end of June 2022.
The symptoms of — such as fatigue, shortness of breath and ‘brain fog’ — can be debilitating. But can you die from long COVID? The answer is not so simple.
How could long COVID lead to death?
There’s still a lot we don’t understand about what causes long COVID. A popular theory is that ‘zombie’ may linger in the body and cause inflammation even after the virus has gone, resulting in long-term health problems. Recent research suggests a reservoir of in the blood might explain why some people experience ongoing symptoms.
We know a serious COVID infection can damage . For example, severe COVID can lead to , persistent heart inflammation, neurological damage and long-term kidney disease.
These issues can in some cases lead to death, either immediately or months or years down the track. But is death beyond the acute phase of infection from one of these causes the direct result of COVID, long COVID or something else? Whether long COVID can directly cause death continues to be a topic of debate.
Of the related to long COVID in the US up to June 2022, the most commonly recorded underlying cause was COVID itself (67.5%). This could mean they died as a result of one of the long-term effects of a COVID infection, such as those mentioned above.
COVID infection was followed by heart disease (8.6%), cancer (2.9%), Alzheimer’s disease (2.7%), lung disease (2.5%), diabetes (2%) and stroke (1.8%). Adults aged 75–84 had the highest rate of death related to long COVID (28.8%).
These findings suggest many of these people died “with” long COVID, rather than from the condition. In other words, long COVID may not be a direct driver of death, but rather a contributor, likely exacerbating existing conditions.

“Cause of death” is difficult to define
Long COVID is a relatively recent phenomenon, so mortality data for people with this condition are limited.
However, we can draw some insights from the experiences of people with post-viral conditions that have been studied for longer, such as myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS).
Like long COVID, is a complex condition which can have significant and varied effects on a person’s physical fitness, nutritional status, social engagement, mental health and quality of life.
Some research indicates people with ME/CFS are at of dying from causes including heart conditions, infections and suicide, that may be triggered or compounded by the debilitating nature of the syndrome.
So what is the emerging data on long COVID telling us about the potential increased risk of death?
Research from 2023 has suggested adults in the US with long COVID were at of developing heart disease, stroke, lung disease and asthma.
Research has also found is associated with a higher risk of (thinking about or planning suicide). This may reflect common symptoms and consequences of long COVID such as sleep problems, fatigue, chronic pain and emotional distress.
But long COVID is more likely to occur in people who have . This makes it challenging to accurately determine how much long COVID contributes to a person’s death.
Research has long revealed in cause-of-death reporting, particularly for people with chronic illness.
So what can we conclude?
Ultimately, long COVID is a that can significantly affect quality of life, mental wellbeing and overall health.

While long COVID is not usually immediately or directly life-threatening, it’s possible it could exacerbate existing conditions, and play a role in a person’s death in this way.
Importantly, many people with long COVID around the world lack access to appropriate support. We need to develop for the optimal management of people with long COVID with a focus on multidisciplinary care.
Dr Natalie Jovanovski, Vice Chancellor’s Senior Research Fellow in the School of Health and Biomedical Sciences at RMIT University, contributed to this article.
, Postdoctoral Research Fellow, School of Health and Biomedical Sciences, ; , Professor and Dean, School of Health and Biomedical Sciences, ; , Vice Chancellor's Senior Research Fellow, ; , Professor of Immunology, , and , Associate Professor, STEM | Health and Biomedical Sciences,
This article is republished from under a Creative Commons licence. Read the .
Victoria's Q3 median ED wait times the lowest on record
Victoria's quarter three performance data (January–March) has shown improvement across...
Irregularities in a clinician's cases prompt 15-month lookback
St Vincent's ���ϳԹ�Ⱥ�� Sydney has detailed a 15-month lookback review — prompted by...
Two researchers receive $899,000 in cardiovascular funding
In heart-related news this Heart Week (5–11 May), two University of Newcastle researchers...








